Sports-Related Brain Injuries - working with Neurology on the Hill
The CNS is working with Neurology on the Hill to update the AAN Position on Sports Concussion:
Position on Sports-Related Brain Injuries: Repetitive Head Impact (RHI), Concussion, Traumatic Encephalopathy Syndrome (TES), and Chronic Traumatic Encephalopathy (CTE)
Background
The American Academy of Neurology (AAN), representing over 36,000 neurology professionals, champions policy measures that ensure the safety and high-quality care of individuals in sports and physical activities. While acknowledging the health benefits of sports, neurologists bring specialized knowledge to the management of neurological injuries athletes may encounter.
Issue Description
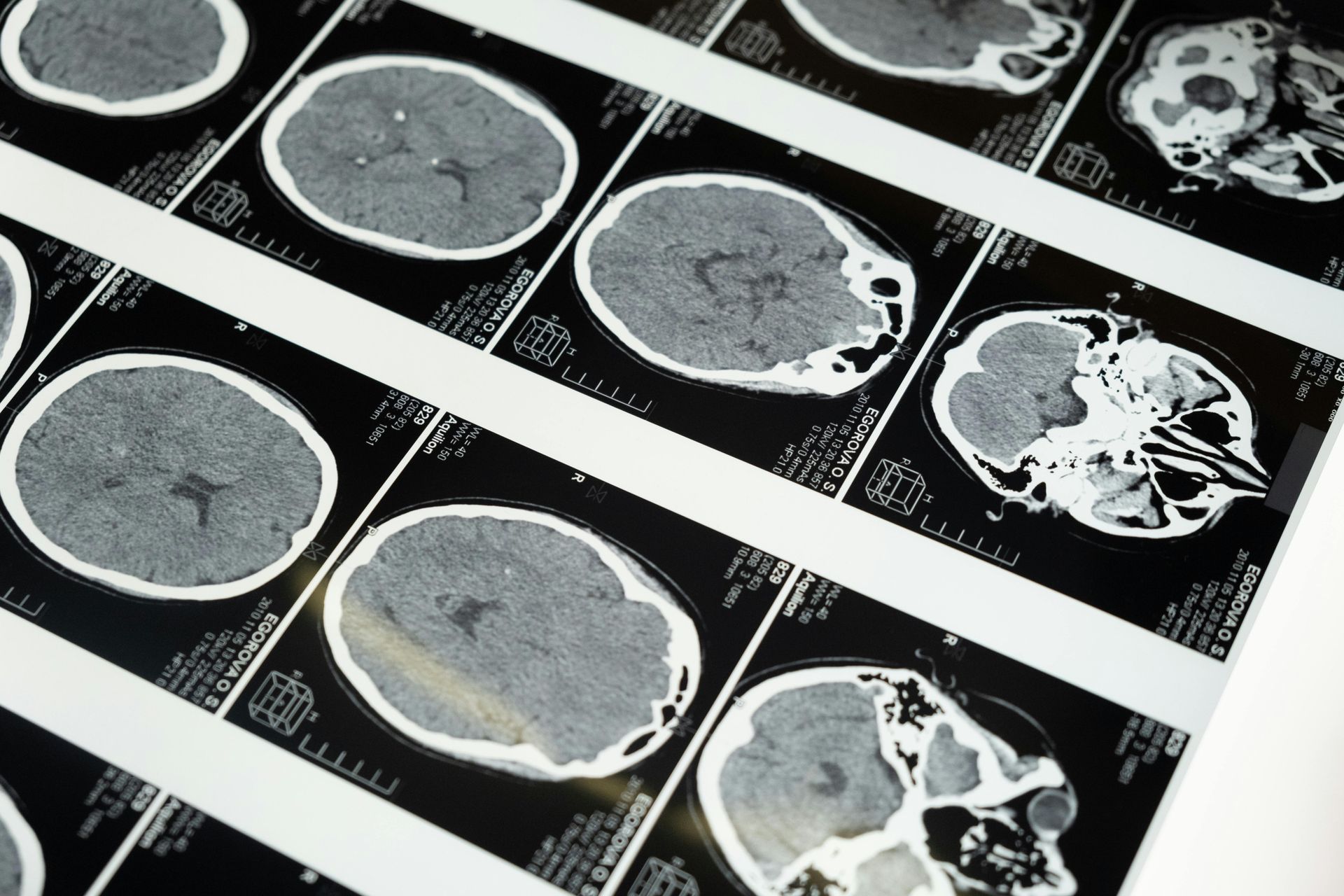
The brain's intricate cellular and fibrous network is susceptible to lasting damage from traumatic brain injuries (TBIs), even those classified as “mild” (mTBI). This vulnerability is featured within a spectrum of injury severity, ranging from Repetitive Head Impact (RHI) and Concussion to Traumatic Encephalopathy Syndrome (TES). Mild TBI can lead to significant long-term neuropathological changes: diffuse axonal injury, demyelination, and Wallerian degeneration. *a Chronic Traumatic Encephalopathy (CTE) is a neurodegenerative condition (tauopathy) identified after death, linked to recurrent traumatic brain injuries. A pathology review of the brains of deceased young athletes across a variety of contact sports disclosed that as many as 42% also met criteria for Chronic Traumatic Encephalopathy (CTE).*b Athletes as young as age 17 have been diagnosed with CTE. *c
Traumatic Encephalopathy Syndrome (TES) - Expanded Insight
Traumatic Encephalopathy Syndrome (TES) *d,e is a critical component of the dialogue on sports-related brain injuries. Characteristically delayed in its clinical presentation, TES is indicative of a complex and progressive neurological condition resulting from repetitive brain injury. The range of symptoms in TES comprise cognitive impairments, mood disorders, behavioral changes, and movement disorders reflecting the enduring consequences of prior repeat concussions and sub-concussive impacts.
TES is intricately linked with CTE. The diagnosis of TES in living patients requires the identification of a delayed emergence of severe symptoms or the progression of milder ones, supported by relevant clinical history. The importance of early detection cannot be overstated, as it enables prompt intervention and advanced management for those at risk of developing TES.
Understanding and addressing TES involves a comprehensive approach that encompasses preventive strategies to minimize head impacts, early detection, and targeted treatments for affected individuals. By focusing on TES as part of the broader spectrum of sports-related brain injuries, healthcare providers, coaches, and policymakers can better protect athletes and support their long-term health and well-being. Incorporating TES awareness into concussion policies and health recommendations is crucial, demanding rigorous pre-participation evaluations, ongoing education on the risks of head impacts, and the adoption of safer sports practices. Supporting research into TES and related conditions is essential for developing effective diagnostics and early interventions, ultimately improving outcomes for those impacted by sports-related brain injuries.
Legislative Actions and Further Recommendations
With Special Considerations for Youth
With a particular focus on youth, legislation nationwide aims to mitigate the adverse effects of sport-related repetitive head impacts and concussions. Given their developing physiology, children are at heightened risk. Therefore, protective measures, such as the prohibition of heading in soccer for children under 12, are imperative. However, protective legislation for young athletes in tackle football remains insufficient. The AAN advocates for legislative action to extend protections, including delaying tackle football participation in our very young. The AAN advocates a safer alternative, flag football for children under 12.
Updating policies to reflect current research is essential for improving concussion and head injury information protocols, standardizing head injury assessment tools, and promoting quality sports brain injury registries, collectively advancing our understanding and management of these injuries and their long-term impact on our youth.
Concussion Policies and Recommendations
The AAN advocates for comprehensive concussion education, the immediate removal from play following a suspected concussion, and a cautious return to play only after clearance by a healthcare provider skilled in concussion management. This protocol applies to organized sports and recreational play alike, emphasizing informed consent, academic support during recovery, and legal protections for healthcare volunteers.
Adopting evidence-based policies is crucial for preventing concussions and their potentially devastating outcomes, significantly reducing the risks associated with sports-related brain injuries.
Conclusion with Emphasis on TES
Addressing Traumatic Encephalopathy Syndrome (TES) in discussions on sports-related brain injuries highlights the need for a nuanced understanding of the long-term effects of repetitive head impacts. Through education, prevention, and research, the neurological health of athletes can be better protected, fostering safer sports environments. Neurologists are key to diagnosing, managing, and researching TES, emphasizing the importance of specialized care and informed policymaking in safeguarding sport athletes.
The American Academy of Neurology (AAN) acknowledges the occurrence of brain injuries in settings beyond athletic activities. This includes military exercises where the nature of training and operational activities can expose individuals to traumatic brain injury (TBI) risks. Brain injuries can also arise from accidents in daily life, occupational hazards, and civil discord. The AAN extends its position to encompass these scenarios, emphasizing the need for awareness, prevention strategies, and appropriate medical responses to brain injuries regardless of their origin. This broad perspective underlines the AAN's commitment to the health and safety of all individuals who might be at risk of brain injuries, not just athletes, highlighting the importance of a comprehensive approach to brain injury prevention, diagnosis, and treatment.
References
Added:
*a Wallerian degeneration as a therapeutic target in traumatic brain injury
Curr Opin Neurol 2019;32(6):786-795
*b Neuropathologic and Clinical Findings in Young Contact Sport Athletes Exposed to Repetitive Head Impacts JAMA Neurol. 2023;80(10):1037-1050
*c The spectrum of disease in chronic traumatic encephalopathy. Brain. 2013;136 :43-64
*d Clinical subtypes of chronic traumatic encephalopathy: literature review and proposed research diagnostic criteria for traumatic encephalopathy syndrome. Alzheimer's Research & Therapy 2014, 6:68
*e NINDS Consensus Diagnostic Criteria for Traumatic Encephalopathy Syndrome
Neurology. 2021;96(18):848-863
Original:
1 Langlois JA, Rutland-Brown W, Wald M. The epidemiology and impact of traumatic brain injury: a brief overview. Journal of Head Trauma
Rehabilitation. 2006;21(5):375-8.
2 Abrahams S, Fie SM, Patricios J, Posthumus M, September AV. Risk factors for sports concussion: an evidence-based systematic review. Br J Sports
Med. 2014 Jan;48(2):91-7.
3 Sarmiento K, Thomas KE, Daugherty J, et al. Emergency Department Visits for Sports- and Recreation-Related Traumatic Brain Injuries Among
Children — United States, 2010–2016. MMWR Morb Mortal Wkly Rep 2019;68:237–242. DOI: http://dx.doi.org/10.15585/mmwr.mm6810a2external icon.
4 DePadilla L, Miller GF, Jones SE, Peterson AB, Breiding MJ. Self-Reported Concussions from Playing a Sport or Being Physically Active Among High
School Students — United States, 2017. MMWR Morb Mortal Wkly Rep 2018;67:682–685. DOI: http://dx.doi.org/10.15585/mmwr.mm6724a3external icon.
5 “Heads Up: Concussion in Youth Sports,” Centers for Disease Control and Prevention. https://www.cdc.gov/headsup/youthsports/index.html
6 McCrory P, Meeuwisse W, Dvorak J, et al. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in
Berlin, October 2016. British Journal of Sports Medicine. 2017; 51:838-847.
7 Harmon KG, Clugston JR, Dec K, et al. American Medical Society for Sports Medicine position statement on concussion in sport. British Journal of Sports Medicine. 2019; 53:213-225.